Did you know that approximately 37.3 million people in the United States have diabetes? This staggering statistic highlights the scale of the impact that diabetes has on our society. When it comes to wound healing, diabetes can pose significant challenges, leading to slow healing, increased risk of infection, and complications such as foot ulcers. Understanding how diabetes affects wound healing is crucial for developing effective strategies to address these issues.
Key Takeaways:
- Diabetes affects approximately 37.3 million people in the United States.
- Diabetes can lead to slow wound healing and increased risk of infection.
- Foot ulcers are a common problem in individuals with diabetes.
- Proper wound care and management of blood glucose levels are crucial for promoting optimal wound healing in diabetics.
- Collaboration with healthcare professionals is essential in developing a personalized treatment plan for individuals with diabetes.
The Challenges of Diabetes Wound Healing
People with diabetes face unique challenges when it comes to wound healing. Due to the nature of the disease, wounds in diabetics often heal slowly or may not heal at all, increasing the risk of complications. One common complication experienced by individuals with diabetes is diabetic foot ulcers. Studies show that approximately 1 in 4 people with diabetes develop foot ulcers, making it a significant concern for healthcare professionals.
Diabetic foot ulcers can have severe consequences if left untreated. They can lead to infections, which can spread rapidly and, in some cases, result in the need for amputation. Managing and treating these ulcers is therefore crucial to prevent further complications and ensure the well-being of individuals with diabetes.
Poor blood glucose control is a contributing factor to the challenges of wound healing in diabetics. Elevated blood glucose levels can hinder the body’s ability to heal wounds effectively. Additionally, impaired immune function is common in individuals with diabetes, further complicating the healing process. Reduced circulation, another common issue among diabetics, can also limit the delivery of essential nutrients and oxygen to the wound site, impeding the healing process.
Effective wound care for diabetics plays a vital role in managing these challenges. It involves proper wound cleaning, appropriate dressing selection, and regular monitoring of the wound’s progress. Adhering to diabetic foot ulcers treatment guidelines can significantly improve outcomes and reduce the risk of complications.
“Diabetic wound management requires a comprehensive approach that addresses all aspects of wound healing, including blood glucose control, infection prevention, and promoting optimal wound environment.”
Key Challenges in Diabetic Wound Healing:
- Slow healing or non-healing wounds
- Increased risk of diabetic foot ulcers
- Potential for serious infections and amputation
- Poor blood glucose control
- Impaired immune function
- Reduced circulation
Addressing these challenges requires a multidisciplinary approach involving healthcare professionals specializing in wound care for diabetics. By understanding the unique complexities of diabetic wound healing, healthcare providers can implement effective strategies to manage wounds, reduce complications, and promote optimal healing.
| Common Challenges in Diabetes Wound Healing | Contributing Factors |
|---|---|
| Slow or non-healing wounds | Poor blood glucose control |
| Increased risk of foot ulcers | Impaired immune function |
| Potential for serious infections and amputation | Reduced circulation |
Acknowledging and addressing the challenges of wound healing in individuals with diabetes is essential for improving outcomes and preventing complications. By implementing proper wound care practices and collaborating closely with healthcare professionals, diabetics can achieve optimal healing and preserve their quality of life.
The Impact of Diabetes on Wound Healing
Uncontrolled diabetes can significantly impair the wound healing process, posing challenges for individuals with diabetes. High blood glucose levels have a detrimental effect on immune function, making it difficult for the body to fight off infections. This places diabetic individuals at a higher risk of developing wound infections.
Furthermore, diabetes can impair circulation, limiting the delivery of essential nutrients to the wound site. Without an adequate supply of nutrients, the wound healing process is slowed down, increasing the time required for complete healing.
In addition to the physical impacts, diabetes can also cause diabetic neuropathy, a condition that leads to reduced sensation in the affected area. As a result, individuals with diabetes may not immediately notice wounds or injuries, leading to delays in seeking treatment. Prompt intervention is crucial in managing wounds effectively and preventing further complications.
Proper wound care is essential in minimizing the risk of infections and promoting the healing process in individuals with diabetes. Following diabetic wound care guidelines can provide valuable insights into wound management techniques. It includes cleansing the wound with mild antiseptic solutions, keeping the wound moist with appropriate dressings, and monitoring for signs of infections such as redness, swelling, or pus formation.
By adhering to these guidelines, individuals with diabetes can take an active role in their wound care and reduce the risks associated with impaired healing. Regular monitoring and assessment by healthcare professionals can ensure that any infections or complications are detected early and treated promptly.
Diabetic Wound Infection
Diabetic wounds are particularly susceptible to infections due to the compromised immune function and impaired circulation associated with diabetes. Infections can lead to more significant complications, such as cellulitis, abscess formation, and even osteomyelitis (bone infection).
Recognizing the signs of a wound infection is crucial in managing diabetic wounds effectively. Some common indicators include increased pain, redness, warmth, swelling, and a foul odor. Any signs of infection should be promptly reported to healthcare professionals for appropriate treatment.
Maintaining good blood glucose control is vital in preventing and managing diabetic wound infections. Elevated blood glucose levels provide an ideal environment for bacterial growth and increase the risk of complications. By keeping blood glucose levels within the target range, individuals with diabetes can significantly reduce the risk of infections and support the healing process.
Diabetic Wound Healing Process
The wound healing process in individuals with diabetes may be complicated and prolonged due to the underlying effects of the disease. Understanding the stages of the healing process can provide valuable insights into managing wounds effectively.
- Hemostasis: This initial stage involves the formation of a blood clot to stop bleeding and create a temporary barrier.
- Inflammation: Inflammation helps clean the wound site, remove debris, and initiate the recruitment of immune cells to fight off infections.
- Proliferation: This stage involves the formation of new tissue, including collagen, granulation tissue, and blood vessels, to fill the wound.
- Remodeling: The final stage focuses on improving the strength and appearance of the healed wound through collagen remodeling and maturation.
Diabetes can disrupt each stage of the wound healing process, leading to delayed or impaired healing. Therefore, appropriate wound care, infection prevention, and management of blood glucose levels are crucial in supporting the diabetic wound healing process.
| Stage | Impact of Diabetes |
|---|---|
| Hemostasis | Diabetes does not significantly impact this stage. |
| Inflammation | Diabetes can delay the recruitment of immune cells and impair their function, prolonging the inflammatory response. |
| Proliferation | Diabetes can impair the formation of new blood vessels and collagen, leading to reduced tissue formation and delayed wound closure. |
| Remodeling | Diabetes can disrupt collagen remodeling and maturation, resulting in weaker scar tissue and an increased risk of wound reopening. |
Understanding the impact of diabetes on the wound healing process can help guide healthcare professionals in developing effective treatment plans tailored to the individual’s needs and promoting optimal healing outcomes.
Mechanisms of Impaired Wound Healing in Diabetes
When it comes to wound healing in individuals with diabetes, chronic inflammation emerges as a key player. Inflammatory cells, including macrophages, experience dysfunction in the presence of elevated blood glucose levels. This dysfunctional inflammation not only contributes to delays in wound closure but also leads to further complications.
Inflammation is a complex biological response that aims to protect the body from harmful stimuli. However, in chronic wounds, inflammation becomes dysregulated and persists for longer periods, hindering the healing process. The persistent inflammation seen in chronic wounds can be attributed to various factors, including the impaired function of inflammatory cells.
Macrophages, a type of immune cell, play a crucial role in wound healing. In individuals with diabetes, macrophages exhibit altered behavior and aberrant inflammatory responses. These dysfunctional macrophages release excessive pro-inflammatory molecules, which contribute to a prolonged inflammatory environment in the wound site. This chronic inflammation interferes with the normal progression of wound healing, leading to delayed healing and increased susceptibility to infections.
Epigenetic mechanisms have also been implicated in the impaired wound healing process observed in diabetes. Epigenetics refers to changes in gene expression that occur without alterations to the DNA sequence. In the context of diabetic wound healing, epigenetic mechanisms such as changes in DNA methylation and histone modification have been observed.
Targeting epigenetic mechanisms holds promise for improving diabetic wound healing. Understanding the epigenetic changes that occur in diabetic wounds can shed light on potential therapeutic targets. By selectively modulating these epigenetic modifications, it may be possible to promote a more favorable wound healing environment and accelerate the closure of diabetic wounds.
Further research is needed to unravel the intricate relationship between inflammation in chronic wounds, inflammation in diabetic wound healing, and the targeting of epigenetic mechanisms. Developing interventions that effectively address these mechanisms has the potential to revolutionize diabetic wound care and improve outcomes for individuals living with diabetes.
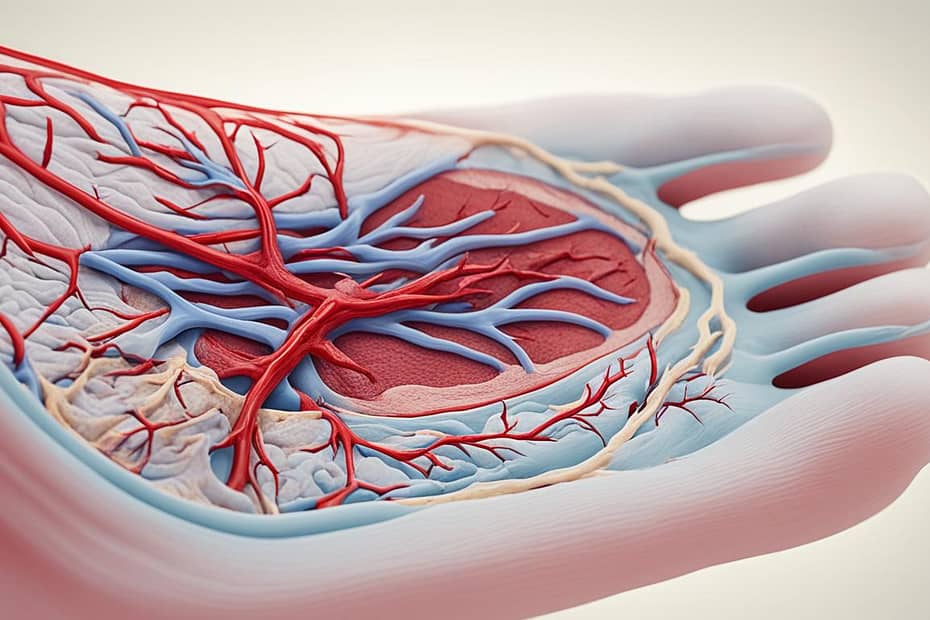
The Role of Angiogenesis in Diabetic Wound Healing
Diabetes can disrupt the process of angiogenesis, which refers to the formation of new blood vessels. Impaired angiogenesis in diabetic wounds can hinder the delivery of oxygen and nutrients to the wound site, **slowing down the healing process**. Understanding the factors that regulate angiogenesis in diabetes is crucial for developing effective strategies to promote wound healing.
Angiogenesis plays a vital role in wound healing by providing the necessary blood supply to support tissue regeneration. In the context of diabetic wounds, **insufficient angiogenesis** can result in **delayed or impaired healing**. This is due to the reduced ability to deliver oxygen, nutrients, and immune cells to the wound site.
Factors such as **elevated blood glucose levels** and **chronic inflammation** in diabetes can negatively affect angiogenesis. High blood glucose levels can interfere with various molecular pathways involved in angiogenesis, disrupting the delicate balance of pro-angiogenic and anti-angiogenic factors. Additionally, chronic inflammation, which is often present in diabetes, can impair the formation of new blood vessels.
To promote angiogenesis and enhance wound healing in individuals with diabetes, several strategies can be employed. These include:
- Effective **blood glucose control** to reduce the negative impact on angiogenesis.
- **Promoting a healthy lifestyle** through regular exercise and a balanced diet, which can support proper blood flow and angiogenic processes.
- Using **advanced wound dressings and biomaterials** that promote angiogenesis and facilitate tissue regeneration.
- **Targeting pro-angiogenic factors** through the use of growth factors or gene therapies to enhance the formation of new blood vessels.
By addressing angiogenesis and implementing these strategies, it is possible to improve the healing outcomes of diabetic wounds. However, further research is needed to fully understand the complex mechanisms underlying angiogenesis in diabetes and develop targeted interventions that promote optimal wound healing.
Image: Angiogenesis in Diabetic Wound Healing
The Impact of Diabetes on Collagen Production
Collagen, the main structural protein in the skin, plays a vital role in wound healing. It provides strength and elasticity to the skin, allowing it to withstand tensile forces during the healing process. However, in individuals with diabetes, collagen production can be disrupted, leading to impaired wound healing.
Diabetes affects collagen production in diabetic wounds in several ways. **Elevated blood glucose levels** can interfere with the synthesis of collagen, hindering its production and reducing its abundance in the wound area. This, in turn, weakens the skin’s structural integrity and impairs the overall wound healing process.
Reduced collagen production in diabetes can have significant consequences for wound closure. Collagen acts as a scaffold for new tissue growth, facilitating the formation of granulation tissue and the re-epithelialization of the wound. When collagen production is compromised, the wound closure process is delayed, resulting in chronic wounds that are more prone to infections and other complications.
Moreover, diabetes-related decreased collagen production can lead to decreased tensile strength in diabetic wounds. Collagen provides the necessary strength and support to withstand mechanical stress. In its absence, the skin becomes more fragile, making it susceptible to further damage and delayed healing.
“The disruption of collagen production in diabetic wounds is a significant contributing factor to the challenges faced in wound healing for individuals with diabetes.”
Managing collagen production is essential for optimizing wound healing in individuals with diabetes. Strategies to promote collagen synthesis, such as optimizing blood glucose control, may help improve collagen production and enhance wound healing outcomes. Additionally, interventions targeting the underlying factors that contribute to reduced collagen production, such as inflammation and impaired angiogenesis, can also be beneficial.
| Factors affecting collagen production in diabetic wounds | Effects on wound healing |
|---|---|
| Elevated blood glucose levels | Interferes with collagen synthesis and reduces collagen abundance |
| Impaired angiogenesis | Reduces the delivery of oxygen and nutrients necessary for collagen production |
| Inflammation | Alters collagen structure and impairs collagen synthesis |
By addressing and managing the factors that disrupt collagen production, healthcare professionals can help improve wound healing outcomes and reduce the risk of complications in individuals with diabetes. Developing personalized treatment plans that target collagen production may lead to better healing rates and improved quality of life for diabetic patients.
The Link Between Diabetes and Infection Risk
Diabetes significantly increases the risk of developing infections in wounds. Individuals with diabetes face unique challenges that make them more susceptible to infections in their wounds. Factors such as **impaired immune function**, **reduced circulation**, and **high blood glucose levels** contribute to this increased risk.
Diabetic foot ulcers are particularly prone to infections, which can have serious consequences if left untreated. The combination of neuropathy, poor blood flow, and high glucose levels creates an ideal environment for bacteria to thrive, increasing the chances of **diabetic wound infection**. These infections can lead to further complications, such as **tissue necrosis** and **cellulitis**.
Proper wound care and **maintaining good blood glucose control** are crucial for preventing infections in individuals with diabetes. Regularly cleaning and dressing wounds, avoiding excessive moisture, and using appropriate antibacterial agents can help reduce the risk of infection. **Regular glucose monitoring** and working closely with healthcare professionals to manage blood sugar levels also play a vital role in minimizing infection risk.
Infection prevention should be a top priority for individuals with diabetes, especially when it comes to managing wounds. By taking proactive measures and following proper wound care guidelines, the risk of developing **diabetic wound infection** can be significantly reduced.
Symptoms of Diabetic Wound Infection
Recognizing the signs of **diabetic wound infection** is crucial in order to seek prompt medical attention. Some common symptoms include:
- Increased pain or tenderness around the wound
- Swelling, redness, or warmth in the surrounding area
- Foul-smelling discharge or pus
- Fever or chills
- Delayed wound healing
If any of these symptoms are present, it is important to seek medical advice as soon as possible. **Early intervention** is key to preventing the spread of infection and reducing the risk of complications.
| Factors Contributing to Infection Risk in Diabetic Wounds | Preventive Measures |
|---|---|
| Impaired immune function | Regular hand washing and vaccination to boost immunity |
| Reduced circulation | Maintaining a healthy lifestyle, including regular exercise |
| High blood glucose levels | Strict blood glucose control through medication, diet, and lifestyle choices |
Strategies to Promote Diabetic Wound Healing
When it comes to promoting wound healing in individuals with diabetes, several strategies can make a significant difference. These approaches encompass maintaining strict blood glucose control, implementing thorough foot care practices, and prompt treatment of wounds. Additionally, there are other interventions, such as growth factors, advanced dressings, and gene therapy, that can provide additional benefits for diabetic wound healing. Collaborating closely with healthcare professionals is essential to develop a personalized treatment plan tailored to each individual’s needs.
Strict blood glucose control plays a crucial role in supporting the healing process of diabetic wounds. Stable blood glucose levels promote optimal wound healing by reducing the risk of complications and facilitating the body’s natural healing abilities. Consistently monitoring blood glucose levels, adhering to prescribed medications, following a balanced diet, and engaging in regular physical activity are essential for effective glucose control and promoting diabetic wound healing.
Thorough foot care is paramount for individuals with diabetes to prevent complications and promote healing. Regularly inspecting the feet for any signs of injury or infection, keeping the feet clean and moisturized, wearing appropriate footwear that provides good support and protection, and avoiding walking barefoot are all crucial aspects of foot care for individuals with diabetes. These practices help reduce the risk of foot ulcers and contribute to overall wound healing.
“Proper wound care is vital for preventing infections and promoting healing.”
Prompt treatment of wounds is critical to prevent further complications. Seeking medical attention as soon as a wound is identified is essential. Healthcare professionals can assess the severity of the wound, clean it properly, and provide appropriate treatment options. This timely intervention minimizes the risk of infection, promotes proper healing, and allows for early identification of any potential issues that may require specialized care.
It is important to remember that wound healing is a complex process, and the right treatment option may vary from person to person. Working closely with healthcare professionals, such as wound care specialists or podiatrists, is crucial in determining the most appropriate treatment plan for optimal diabetic wound healing.
Interventions for Diabetic Wound Healing
| Treatment Options | Description |
|---|---|
| Growth Factors | These substances promote tissue regeneration by stimulating cell growth and migration. |
| Advanced Dressings | Specialized dressings can facilitate wound healing by providing a moist environment, promoting debridement, and preventing infection. |
| Gene Therapy | This cutting-edge approach aims to enhance wound healing by introducing specific genes into cells to promote tissue regeneration and reduce inflammation. |
The image above illustrates the importance of holistic approaches, such as strict blood glucose control, foot care practices, and prompt wound treatment, in promoting diabetic wound healing.
By implementing these strategies and working collaboratively with healthcare professionals, individuals with diabetes can enhance their wound healing potential and minimize the risks associated with diabetic foot ulcers and other wounds. Remember, proper wound care is essential for preventing infections and facilitating healing, leading to better long-term outcomes.
The Importance of Glucose Control in Diabetic Wound Healing
Effective glucose control plays a crucial role in promoting optimal wound healing in individuals with diabetes. Poor management of blood glucose levels can have negative consequences on the healing process, leading to delayed wound closure, increased infection risk, and other complications.
Monitoring blood glucose levels regularly is essential for maintaining stability and supporting the healing process. It allows individuals to take timely action to adjust their treatment plan, ensuring that their blood glucose remains within the target range. This proactive approach helps to minimize the impact of high blood glucose levels on the wound healing process.
Alongside regular monitoring, adhering to prescribed medications and following a balanced diet are equally vital for glucose control in diabetes. Medications, such as insulin or oral hypoglycemic agents, help regulate blood glucose levels and maintain stability throughout the healing process. A balanced diet that includes a good mix of complex carbohydrates, proteins, and healthy fats can aid in maintaining stable blood glucose levels and provide the necessary nutrients for wound healing.
“Maintaining stable blood glucose levels is like providing the ideal environment for wound healing to occur. It minimizes the risk of complications and ensures a smoother healing process.”
Physical activity and glucose control
Regular physical activity is another crucial component of effective glucose control in diabetes. Engaging in aerobic exercises, such as brisk walking, swimming, or cycling, helps improve insulin sensitivity and assists in regulating blood glucose levels. It also promotes better circulation, allowing essential nutrients and oxygen to reach the wound site, thereby enhancing the healing process.
However, it is essential to consult with a healthcare professional before starting any new exercise regimen. They can provide personalized recommendations and guidance based on an individual’s specific needs and medical condition.
The impact of glucose control on wound healing
Proper glucose control has a significant impact on wound healing in individuals with diabetes. When blood glucose levels are well-managed, the risk of infection decreases, and the body’s immune response remains strong. This enables the body to efficiently fight off bacteria and other pathogens, reducing the likelihood of complications.
In addition to infection prevention, glucose control supports the normal healing process by promoting collagen synthesis and angiogenesis. Collagen, a vital component of wound healing, is produced more efficiently when blood glucose levels are stable. Similarly, stable blood glucose levels encourage the formation of new blood vessels, boosting the delivery of oxygen and nutrients to the wound site.
Overall, maintaining proper glucose control helps create an ideal environment for wound healing, minimizing complications, and accelerating the healing process.
Image: Glucose control is vital for promoting optimal wound healing in individuals with diabetes.
Prevention and Early Intervention in Diabetic Wound Healing
Preventing complications is key in diabetic wound healing. By prioritizing regular foot care, maintaining good blood glucose control, and seeking prompt treatment for any wounds that do develop, individuals with diabetes can minimize the risk of diabetic wound complications. Regular check-ups with healthcare professionals, such as podiatrists and wound care specialists, play a crucial role in this process. These professionals can identify potential issues early on and implement appropriate interventions to prevent them from progressing.
Educating individuals with diabetes about the risks and proper care of diabetic wounds is also essential for effective prevention and early intervention. By understanding the importance of meticulous foot hygiene, recognizing the signs of potential complications, and knowing when to seek medical attention, individuals can take proactive steps to minimize the impact of diabetic wounds on their overall health and well-being.
By combining diligent self-care practices with professional guidance, individuals with diabetes can empower themselves to take control of their wound healing journey. With a proactive approach to prevention and early intervention, the risk of diabetic wound complications can be significantly reduced, leading to improved outcomes and better quality of life.
Conclusion
In summary, it is evident that diabetes has a profound impact on wound healing. Slow healing, increased infection risk, and other complications are common in individuals with diabetes. To promote optimal wound healing, proper management of blood glucose levels is crucial. By diligently monitoring and controlling blood glucose, individuals can minimize delays in wound closure and reduce the risk of infections and other complications.
Equally important is diligent wound care. Regularly cleaning wounds, applying appropriate dressings, and seeking prompt medical attention for any issues that arise are vital steps in ensuring successful wound healing. Early intervention is key, as it can prevent minor wounds from developing into major problems.
To achieve the best outcomes for wound healing, individuals with diabetes should work closely with healthcare professionals. Developing a personalized treatment plan that addresses their specific needs and risk factors is essential. By taking a proactive approach and following the guidance of healthcare experts, individuals with diabetes can overcome the challenges associated with wound healing and achieve optimal recovery.
FAQ
How does diabetes impact wound healing?
What are the challenges of wound healing in individuals with diabetes?
How does diabetes impair the wound healing process?
What mechanisms contribute to impaired wound healing in diabetes?
How does diabetes affect angiogenesis in wound healing?
What is the impact of diabetes on collagen production?
Why are individuals with diabetes at higher risk of infections in wounds?
What strategies can promote diabetic wound healing?
Why is glucose control important in diabetic wound healing?
How can complications in diabetic wound healing be prevented?
How does diabetes impact wound healing overall?
Source Links
- https://www.medicalnewstoday.com/articles/320739
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8432997/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7243111/