Did you know that an estimated 19 million people worldwide had clinically significant Diabetic Macular Edema (DME) in 2020? That number is projected to rise to over 28 million by 2045. DME is a complication of diabetes that affects the macula, the area responsible for detailed vision in the retina.
When left untreated, DME can cause vision loss and significantly impact daily life. However, with early detection and proper treatment, vision loss can be prevented. Understanding the symptoms, diagnosis, and available treatment options for DME is crucial for managing this condition effectively.
Key Takeaways:
- Diabetic Macular Edema (DME) is a complication of diabetes that affects the macula, causing vision problems.
- Early detection through regular eye exams is crucial for preventing vision loss in DME.
- Treatment options for DME include anti-VEGF injections, laser surgery, corticosteroids, and NSAID eyedrops.
- Managing systemic diseases like diabetes, hypertension, and hyperlipidemia can delay the progression of DME.
- Prevention strategies for DME involve maintaining good diabetes control and regular eye screenings.
In the following sections, we will delve deeper into the understanding, symptoms, diagnosis, risk factors, treatments, prevention, and prognosis of Diabetic Macular Edema.
Understanding Diabetic Macular Edema
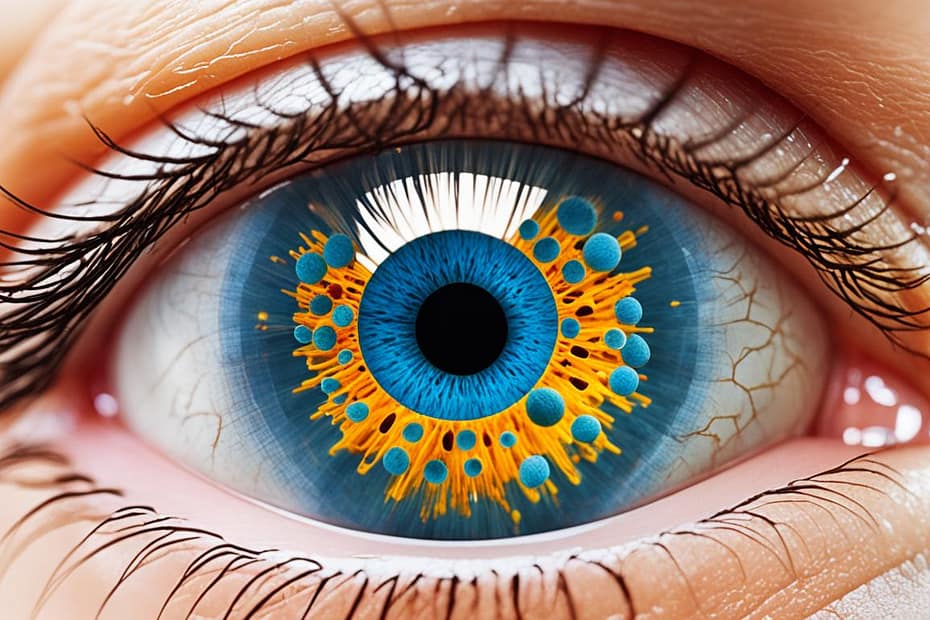
Diabetic macular edema (DME) is a complication of poorly controlled diabetes that affects the macula, a small area at the center of the retina responsible for detailed vision. DME occurs when fluid, protein, and lipids accumulate in the retina, leading to retinal microvascular obstruction and capillary dropout. This process is caused by retinal ischemia, a condition where the blood supply to the retina is compromised.
Retinal ischemia triggers the upregulation of proinflammatory cytokines, which promote inflammation and result in the loss of vascular pericytes. This loss compromises the integrity of the microcapillaries in the macula, leading to leakage and the formation of intraretinal cystic spaces. The accumulation of fluid, protein, and lipids causes retinal thickening, the presence of hard exudates, and edema within the macula, all of which are characteristic features of DME.
DME can significantly impact visual acuity and quality of life for individuals with diabetes. It is important to note that DME is not exclusive to patients with diabetic retinopathy and can occur independently. However, it is more prevalent in patients with diabetic retinopathy, a condition characterized by progressive damage to the blood vessels in the retina due to diabetes.
“The accumulation of fluid, protein, and lipids causes retinal thickening, the presence of hard exudates, and edema within the macula, all of which are characteristic features of DME.”
The complex pathophysiology of DME involves interplay between various factors, including retinal microvasculature, retinal ischemia, neovascularization, proinflammatory cytokines, and vascular permeability. Understanding these mechanisms is crucial for developing effective treatment strategies and optimizing patient outcomes.
Symptoms and Diagnosis of Diabetic Macular Edema
Symptoms of diabetic macular edema (DME) can vary in severity, ranging from mild blurred vision to severe loss of central vision. Individuals with DME may also experience other visual changes that can be concerning, such as:
- Increased eye floaters
- Washed-out colors
- Dark spots
- Bent or curved lines
- Difficulty seeing in bright light
- Objects appearing wavy or different sizes
It is important to note that these symptoms can also be associated with diabetic retinopathy, a common complication of diabetes that can lead to DME. Therefore, it is crucial for individuals experiencing these visual changes to seek medical attention for a comprehensive eye examination.
Diabetic macular edema is typically diagnosed through various diagnostic tests, including nonmydriatic retinal photography and optical coherence tomography (OCT).
Nonmydriatic retinal photography involves capturing images of the retina using a specialized camera without the need for dilating the pupils. This method can provide detailed images of the macula, allowing healthcare professionals and artificial intelligence algorithms to detect any signs of DME.
Optical coherence tomography, on the other hand, is a non-invasive imaging test that uses light waves to create cross-sectional images of the retina. This technology assists in assessing retinal thickness and identifying the presence of edema in individuals suspected of having DME.
By combining these diagnostic approaches, healthcare professionals can accurately diagnose and monitor the progression of diabetic macular edema, enabling them to develop appropriate treatment plans.
Risk Factors and Prognosis of Diabetic Macular Edema
When it comes to diabetic macular edema (DME), understanding the risk factors and prognosis is crucial for effective management and prevention of vision loss. Several factors contribute to the development of DME, including:
- Diabetes Duration: Individuals with long-standing diabetes are at a higher risk of developing DME.
- Blood Sugar Control: Poor management of blood sugar levels increases the likelihood of DME.
- High Blood Pressure: Hypertension is a significant risk factor for DME.
- Kidney Disease: Individuals with kidney disease are more prone to developing DME.
- High Cholesterol: Elevated cholesterol levels are associated with an increased risk of DME.
- Tobacco Use: Smoking and tobacco consumption exacerbate the risk of DME.
- Ethnicity: African Americans and Hispanics have a higher susceptibility to DME.
If left untreated, DME can cause irreversible damage to the macula, leading to permanent vision loss. However, early detection, timely intervention, and long-term follow-up care can significantly impact the prognosis. By effectively managing systemic diseases such as diabetes, hypertension, and hyperlipidemia, the progression of DME can be delayed, preserving vision and improving outcomes.
To better understand the risk factors and the effectiveness of treatment, let’s take a closer look at some data:
| Risk Factors | Percentage of Diabetic Macular Edema Cases |
|---|---|
| Diabetes Duration | 73% |
| Blood Sugar Control | 58% |
| High Blood Pressure | 62% |
| Kidney Disease | 41% |
| High Cholesterol | 37% |
| Tobacco Use | 28% |
| Ethnicity | 29% African Americans, 26% Hispanics |
As seen in the data, certain risk factors play a significant role in the prevalence of DME. Effective management of these risk factors through medication, lifestyle changes, and regular monitoring can improve the prognosis and prevent further deterioration of vision.
Treatments for Diabetic Macular Edema: Anti-VEGF Injections
Anti-VEGF injections are a common treatment option for patients with diabetic macular edema (DME). These injections play a crucial role in blocking the protein VEGF, which is responsible for the abnormal growth of blood vessels and vascular leakage in the retina. By inhibiting VEGF, anti-VEGF shots help reduce macular edema and preserve vision.
There are several medications used as anti-VEGF treatments for DME, including:
- Aflibercept: This medication acts as a VEGF-A and placental growth factor (PlGF) antagonist, effectively inhibiting abnormal blood vessel formation and leakage in the retina.
- Bevacizumab: A widely used anti-VEGF therapy in ophthalmology, bevacizumab works by binding to VEGF and inhibiting its effects on blood vessel growth.
- Ranibizumab: Similar to bevacizumab, ranibizumab is also an anti-VEGF medication that helps reduce vascular leakage and improve vision in patients with DME.
- Faricimab-svoa: This novel anti-VEGF/Ang-2 inhibitor has shown promising results in clinical trials, demonstrating its efficacy in inhibiting both VEGF and Ang-2 to provide improved outcomes for individuals with DME.
Anti-VEGF injections are typically administered via a thin needle directly into the center of the eye. The procedure is performed in an ophthalmologist’s office and usually requires monthly treatments to maintain the benefits of the therapy.
These anti-VEGF treatments not only block VEGF, but some also inhibit Ang-2, which stabilizes fragile new blood vessels and reduces their sensitivity to VEGF effects. This dual inhibition mechanism helps to further restrain abnormal blood vessel growth and leakage in the retina, providing significant benefits for individuals with DME.
“Anti-VEGF injections are a breakthrough in the treatment of diabetic macular edema, offering targeted therapy that directly addresses the underlying causes of the condition.”
While anti-VEGF injections have revolutionized the management of DME, it’s important to note that individual treatment plans may vary depending on the severity of the condition and the patient’s overall health. Therefore, it is crucial for patients to consult with their ophthalmologist to determine the most suitable treatment approach for their specific needs.
Treatments for Diabetic Macular Edema: Laser Surgery and Corticosteroids
When it comes to treating diabetic macular edema (DME), there are several options available. Two common treatments are laser surgery and corticosteroids.
Laser Surgery: Focal-Grid Macular Laser Surgery
Laser surgery, specifically focal-grid macular laser surgery, is a procedure that can help seal leaking blood vessels and slow the growth of new vessels in DME. By targeting specific areas of the macula, this surgery can reduce leakage and swelling, ultimately protecting central vision.
During the procedure, a laser is used to create small burns in the affected areas of the retina. These burns cause the abnormal blood vessels to shrink and seal off, preventing further leakage into the macula. Focal-grid macular laser surgery is typically performed as an outpatient procedure and does not require a hospital stay.
Corticosteroids: Decreasing Inflammation and Swelling
Another treatment option for DME is the use of corticosteroids. Corticosteroids can help decrease inflammation and swelling in the retina, which can improve symptoms and prevent further vision loss. These medications can be administered through an injection or as a sustained-release implant.
Injected corticosteroids are delivered directly into the eye, targeting the affected area. The injection is typically performed in a clinic or doctor’s office and may require local anesthesia. Sustained-release implants, on the other hand, are small devices that are surgically placed in the eye. These implants slowly release medication over time, providing a longer-lasting effect.
It’s important to note that while corticosteroids can be effective in treating DME, they do come with potential risks. Prolonged use of corticosteroids can increase the risk of cataracts and glaucoma. Therefore, corticosteroids may be considered as an alternative treatment option for patients who do not respond well to anti-VEGF therapy or who have specific contraindications to other treatments.
Utilizing laser surgery and corticosteroids can be valuable treatments for diabetic macular edema. Whether it’s sealing leaking blood vessels or reducing inflammation and swelling, these interventions play a crucial role in managing DME and preserving vision.
Treatments for Diabetic Macular Edema: NSAID Eyedrops
Nonsteroidal anti-inflammatory drugs (NSAIDs), in the form of eyedrops, are a viable option for the prevention and management of Diabetic Macular Edema (DME). Unlike steroids, NSAID eyedrops effectively combat inflammation without the same undesirable side effects.
For individuals who cannot or prefer not to take steroids to reduce swelling, NSAID eyedrops provide a safer alternative. Whether administered before or after eye surgery, these eyedrops help in preventing the occurrence or worsening of DME. NSAID eyedrops are often prescribed as an alternative treatment for individuals who are unsuitable candidates for steroids.
How Do NSAID Eyedrops Work?
NSAID eyedrops work by inhibiting the production of prostaglandins, which are responsible for swelling and pain associated with inflammation. By reducing inflammation in the eye, these eyedrops help alleviate symptoms of DME such as swelling and improve visual acuity.
Potential Benefits of NSAID Eyedrops:
1. Anti-inflammatory action: NSAID eyedrops effectively reduce inflammation in the eyes.
2. Swelling reduction: These eyedrops assist in controlling swelling caused by DME.
3. Improved visual acuity: By addressing inflammation and swelling, NSAID eyedrops can enhance visual clarity in individuals with DME.
NSAID eyedrops provide a safer alternative to steroids, offering effective anti-inflammatory action without the associated side effects.
It is important to remember that while NSAID eyedrops can be beneficial, the decision to use them as a treatment for DME should be made in consultation with a qualified healthcare professional. They will be able to assess individual circumstances and recommend the most appropriate treatment approach based on specific needs and conditions.
| Advantages of NSAID Eyedrops | Disadvantages of NSAID Eyedrops |
|---|---|
| – Effective anti-inflammatory action – Suitable alternative to steroids – Control swelling – Improved visual acuity |
– Potential for eye irritation – Allergic reactions in some individuals – Not suitable for all patients with DME |
Prevention of Diabetic Macular Edema
To avoid the complications of diabetic macular edema (DME), it is essential to prioritize preventive measures. Regular eye exams and screenings play a crucial role in early detection and intervention, especially for high-risk individuals. Pregnant women with diabetes should undergo eye exams as soon as possible to detect any potential problems that might arise during pregnancy.
Managing diabetes effectively is a key component of DME prevention. By maintaining good diabetes control, individuals can help delay or even prevent the onset of DME. This includes diligently monitoring blood sugar levels, adhering to prescribed medication regimens, and adopting a healthy lifestyle. Controlling other risk factors such as blood pressure and cholesterol levels is also important in reducing the risk of developing DME.
One of the advantages of regular eye exams is the ability to detect changes in the eyes that indicate the early stages of diabetic retinopathy. Even before symptoms of DME appear, an eye doctor can identify these changes and recommend appropriate interventions. Early detection is vital for preserving vision and preventing permanent damage caused by DME.
In conclusion, preventing diabetic macular edema requires proactive steps such as regular eye exams, screenings, and comprehensive diabetes management. By prioritizing vision health and taking preventive measures, individuals can potentially avoid the complications and vision loss associated with DME.
Epidemiology of Diabetic Macular Edema
Diabetic macular edema (DME) is a prevalent condition affecting millions of people worldwide. In 2020 alone, an estimated 19 million individuals were diagnosed with clinically significant DME. Unfortunately, the prevalence is predicted to rise significantly to over 28 million by 2045, highlighting the urgent need for effective management and prevention of this condition.
Within the United States, DME is a significant concern, particularly amongst adults aged 40 and older with diabetes. It is estimated that approximately 3.8% of this population has DME, emphasizing the impact of the condition on public health.
Notably, certain demographic groups face a higher risk of developing diabetic macular edema. Black Americans, for instance, exhibit both a higher incidence of diabetes and a greater likelihood of developing DME compared to white, non-Hispanic adults. This disparity underscores the importance of targeted interventions and equitable access to healthcare services for vulnerable populations.
Worldwide Statistics
The worldwide prevalence of DME reflects the global burden of diabetes and its associated complications. As diabetes rates continue to rise, so does the incidence of DME. It is a pressing public health concern that demands comprehensive strategies for prevention, early detection, and treatment.
US Statistics
Within the United States, the increasing prevalence of DME highlights the necessity for better disease management and intervention strategies. Improving diabetes control and expanding access to regular eye examinations are crucial steps towards reducing the burden of DME in the country.
img {
display: block;
margin-left: auto;
margin-right: auto;
width: 50%;
}
Conclusion
Diabetic macular edema (DME) is a significant complication of diabetes that can lead to vision loss if left untreated. Fortunately, there are several effective treatment options available to slow the progression of DME and preserve vision.
Treatments such as anti-VEGF injections, laser surgery, corticosteroids, and NSAID eyedrops have been proven to be successful in managing DME. These interventions target the underlying causes of vision loss and help reduce the severity of macular edema.
Prevention plays a crucial role in managing DME. Regular eye exams and screenings, along with maintaining good diabetes control, are essential for early detection and intervention. By monitoring blood sugar levels and managing systemic diseases, individuals can minimize the risk of developing DME and prevent permanent damage to the macula.
Long-term follow-up care and management of systemic diseases are key to improving the prognosis of diabetic macular edema. By working closely with healthcare professionals, individuals can effectively manage DME and maintain their visual health for the long term.
FAQ
What is diabetic macular edema (DME)?
What are the risk factors for diabetic macular edema?
How is diabetic macular edema diagnosed?
What are the treatment options for diabetic macular edema?
How can diabetic macular edema be prevented?
What is the prognosis of diabetic macular edema?
Source Links
- https://www.webmd.com/diabetes/diabetic-macular-edema-treatment
- https://www.everydayhealth.com/diabetic-macular-edema/
- https://www.aao.org/eyenet/article/diabetic-macular-edema-diagnosis-and-management